How Surgical Delays Affect the Bottom Line
Nowhere in the hospital is this drive for cost containment and increased patient volume more evident than in the operating theatre. Here, costs are measured in minutes and revenue gained on a per case basis.1
–J.A. Girottoet al.
International Journal of Surgery
OR time delays are critical to the profitability of each patient case. Taken together, seemingly small delays can result in profit erosion for your entire hospital. Implementing small changes to avoid or eliminate delays can have a direct and positive impact on your bottom line.
The Economics of OR Margin
Approximately 65% of all hospital admissions are due to surgical interventions and account for more than 40% of the total expenses of a hospital.2Each surgical facility needs a clear understanding of its economic structure to establish the groundwork for an efficient and well-functioning OR suite. Underlying the concern for the cost of OR time is another issue: “How much money is being lost through delays?”.3
In today’s climate of Value-based Reimbursement,providers’ payments are based on the “value of care” delivered to treat a patient during a specific episode of care. Your hospital’s overall financial success now depends on cost containment to protect margins while delivering the best patient experience possible. Understanding and mitigating “cost leaks” in your OR is a high-return place to start.
Non-profit Total Knee Replacements?
Are you giving away your profits through time delays in the most valuable real estate in your hospital?
The impact on margin will vary greatly depending on each facility’s specific costs, charges, and reimbursement, but when you consider that over 61%2 of all surgical procedures experience a delay, you may be essentially giving away your profit margin without realizing it.
Let’s look at an inpatient total knee replacement without major complications. If, for example, yours is one of the many hospitals participating in Medicare’s Comprehensive Care for Joint Replacement (CCJR) bundled payment model, your Medicare payment for the complete bundle of care could range from $18,000 to $33,000.4
Using an average Medicare payment of $25,5005 and applying an historical average hospital operating margin of 6%6 would yield approximately $1,530 of profit per episode:
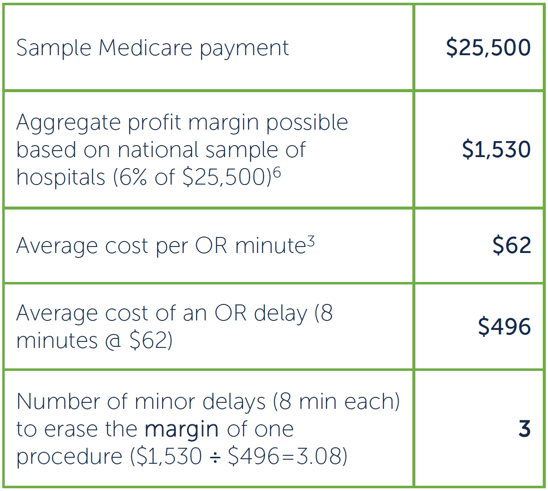
For every 3 procedures with a delay, you're giving one away at cost!
There are always challenges to running a busy OR, so seemingly small delays can be dismissed as being the normal course of cases, or you can look at any delay as an opportunity to improve.
Take Steps to Reduce Delays and Protect Margins in Each Surgical Procedure
- Document your delays to understand root causes, and analyze trends.
- Calculate your costs per procedure.
- Identify your facility’s current margins by procedure.
- Understand the top delays for each procedure and the time lost per delay.
- Review product selection and workflow, including asset tracking and staff tracking.
- Identify areas for improvement and implement an action plan for each.
- Set a measurable goal to improve margins for each procedure and monitor progress.
- Involve everyone and communicate successes!
Small Changes, Big Impact
At an average of $62 per minute3, even small delays can add up quickly. Yet many common delays in the OR can be minimized with simple changes. Halyard suggests some ways you can address these “pain points” in three categories:
Product
Pain Point: Strikethrough on gowns or face masks resulting from wearing the wrong protection-level for the procedure.
Time Impact: 10 – 15 Minutes to break scrub, rescrub, replace mask, re-gown and re-glove.
Cost of Delay: $620 – $930
Halyard Solution: With AERO SERIES* gowns from Halyard, the color difference makes it easy to choose between AAMI Level 3 protection (for most procedures) and AAMI Level 4 for longer, high-fluid procedures. Similarly, FLUIDSHIELD* ASTM-rated surgical masks help wearers choose the appropriate level of facial protection.
Pain Point: Tears in sterilization wrap or damaged instrument containers that require replacement sets or re-sterilization.
Time Impact: 8 – 60 Minutes for flash sterilization or up to an hour to obtain a terminally-sterilized replacement set.
Cost of Delay: $496 – $3,720
Halyard Solution: SMART-FOLD* Sterilization wrap is 61% heavier, with reinforced zones around tray corners and edges.
Facility
Pain Point: Critical equipment or implants not ready or not available to start the procedure.
Time Impact: 10 Minutes to hours to locate and prep required equipment.
Cost of Delay: $620 – $$$$
Halyard Solution: AiRISTA® Equipment tracking and monitoring systems let you easily locate critical products and equipment to be sure they arrive at the OR when needed.
Staff
Pain Point: Surgical team members or patients are not ready, not available or need to leave during the procedure. Work will stop (or not start) until the team is complete and ready.
Time impact: 10 Minutes to hours
Cost of delay: $620 – $$$$
Halyard Solution: AiRISTA® Staff and patient tracking systems tell you where your patient and OR team members are (and where they’re scheduled to be) so that you can confidently plan for each procedure.
REMEMBER: Every minute counts and it only
takes an OR Minute to Lose Your Margin!
Addressing OR delays is one of the more productive opportunities to decrease costs and increase profits in your facility. Contact your Halyard representative for assistance in developing OR time savings solutions that fit your OR. For more information on Halyard surgical products and technologies go to:
Sources
- 1. Girotto, J A., et al. Optimizing your operating room: Or, why large, traditional hospitals don’t work. International Journal of Surgery. 2010; 8(5): 359-67. Available from: 1743919110000804
- Van Winkle, Rachelle A., et al. Operating Room Delays: Meaningful Use in Electronic Health Record, CIN: Computers, Informatics, Nursing. 2016:1. Available from: le_article.pdf
- Macario, Alex, What does one minute of operating room time cost? J Clin Anes. 2010; 22: 233-36. Available from: ment2.pdf
- Average of Medicare expenditures for surgery, hospitalization, and recovery from 2014 ranging from $16,500 to $33,000 per episode. Centers for Medicare & Medicaid Services, Comprehensive Care for Joint Replacement Model. Available from: https://innovation.cms.gov/initiatives/cjr
- Richter DL and Diduch DR. Cost Comparison of Outpatient Versus Inpatient Unicompartmental Knee Arthroplasty. Ortho J Sports Med. 2017 Mar;5(3), 2.
- Hayford T, Nelson L, Diorio A.. Projecting Hospitals’ Profit Margins Under Several Illustrative Scenarios, Working Paper Series 2016-04, Congressional Budget Office, pp. 16-17. Available from 2015-2016/workingpaper/51919- Hospital-Margins_WP.pdf