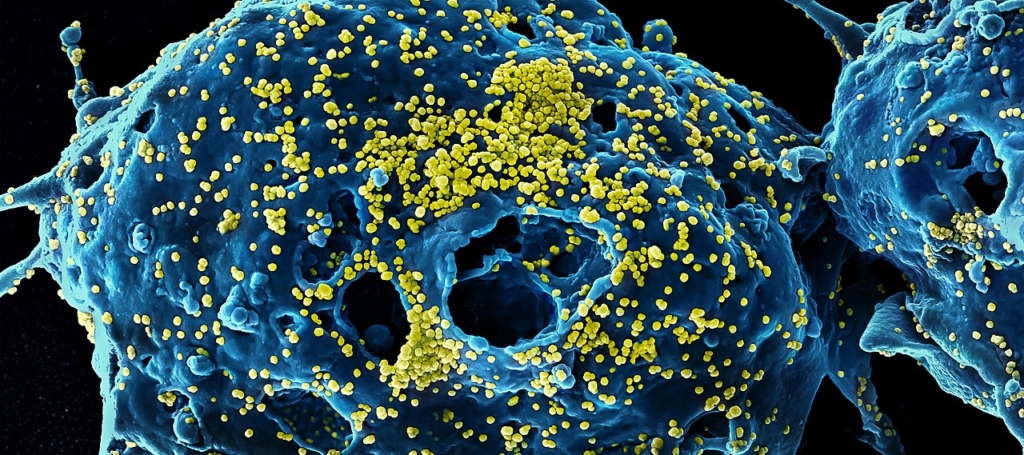
Hospitals are charged with the difficult task of accepting and treating sick patients while aiming to maintain an environment that prevents the spread of infection to other patients, staff and visitors. The task is not an easy one, and the risks are serious. If hospital staff don’t follow infection prevention protocols, it increases the chances of patients getting a healthcare-associated infection (HAI). According to Centers for Disease Control and Prevention (CDC), on any given day, about one in 31 hospital patients has at least one HAI. That amounts to roughly 2 million patients a year, 90,000 of whom die.
Cross-contamination is most often thought of around infections/HAIs, but can mean other risks to patients, including exposure to medications that may be harmful.
There are some obvious areas at risk for cross-contamination, including commonly touched surfaces like bedrails, over-the-bed tables, commodes, doorknobs and faucets. Additionally, equipment that travels around hospital units, such as crash carts, various imaging devices such as EKGs and portable ultrasounds, and food trays, can pose contamination risk if disinfection protocols are not consistently and accurately followed.
Cross-contamination can also entail the transfer of medications from one patient to another.
Cross-contamination can happen with less-thought-of equipment such as pill-cutters, splitters and crushers, which, if not properly cleaned in between uses, can cause a patient to receive traces of a previous patient’s medication. This can be particularly harmful in the cases of medications that have the ability to cause allergic reactions, such as penicillin. The Joint Commission standard MM.05.01.07, which focuses on medication preparation, includes the use of pill splitters. In 2017, MM.05.01.07 violations were the fourth most common Joint Commission violation, accounting for 14.15%.
Working to identify potential areas at risk for cross-contamination and establishing practices and protocols to mitigate those risks can help to increase safety for patients and staff alike. Here are a few best practices to follow:
- Practice stellar hand hygiene: When it comes to keeping patients safe and reducing HAIs, practicing proper hand hygiene is critical. There is much scientific evidence showing that microbes causing HAIs are most frequently spread via the hands of healthcare workers. Be sure to train workers on when to practice hand hygiene, techniques to do it properly as well as displaying written statements that indicate the value.
- Follow cleaning and disinfecting protocols: The CDC outlines very specific environmental infection control guidelines, which include how to properly disinfect and clean surfaces—all staff should be knowledgeable about and confident in their role in adhering to these guidelines as an organization. In addition to critical items such as endoscopes, be sure to pay attention to other patient care items as well, including bed pans, blood pressure cuffs, crutches and computers. These may be decontaminated in the environment they are used and do not require a trip to central processing.
- Use proper personal protective equipment (PPE): In addition to practicing proper hand hygiene, it is important for healthcare workers to wear the appropriate PPE for the task at-hand. These can include a number of different combinations of gloves, masks, eye protection and gowns. In the case of gloves, to further mitigate risk to both staff and patients be sure to follow established protocols and inform staff of their potential limitations. These include:
- Contamination can occur as a result of small, undetectable holes in the gloves
- Contamination may occur during removal of gloves
- Wearing gloves does not replace the need for proper hand hygiene
- Failure to remove gloves after caring for a patient may lead to transfer of microorganisms to subsequent patients
- Consider single-use products when possible: In certain instances, there are single-use products that are disposed of after treating one patient that can help reduce the risk of cross-contamination. Some, such as gloves, are more obvious than others. Examples where less-common items healthcare facilities can consider purchasing in single-use are pill cutters, splitters and crushers, as well as blood pressure cuffs. According to the CDC, “when contact precautions are indicated for patient care, use disposable patient-care items (e.g. blood pressure cuffs) whenever possible to minimize cross-contamination with multiple-resistant microorganisms.”
Though there are sometimes elements outside of our control in patient care, making every effort to protect the safety of those within healthcare facilities is well within our reach. Considering both the common—and even less common—risks for cross-contamination in your facility and establishing protocols and corresponding education to mitigate them, is an important aspect of ensuring the health and well-being of your staff, patients and the loved ones who come to visit them.