At its core, a cleanroom is a specialized area of a facility that requires a strict contamination control strategy. This means the amount and concentration of airborne particles is controlled and classified, and that the room is designed, constructed and operated in a manner to regulate the introduction, generation and retention of particles1. Given the highly regulated nature of cleanrooms, the ability to maintain how a cleanroom is controlled and monitored is critical. Even trace amounts of particles can cause contamination in a cleanroom and potentially lead to a production shut down.
There are two main processes for cleanroom maintenance and control – sterile and aseptic. For a cleanroom to be sterile, it must be free of all living microorganisms. To achieve this, sterile processes use physical or chemical procedures to destroy all microorganisms, including large numbers of resistant bacteria spores2. Aseptic processes do not create a sterile environment but maintain product sterility and prevent contamination from microorganisms2. For cleanrooms, this means keeping everything inside the environment free from contamination. While the two processes have characteristics that overlap, they are not interchangeable and appropriately utilizing both is key for proper cleanroom maintenance.
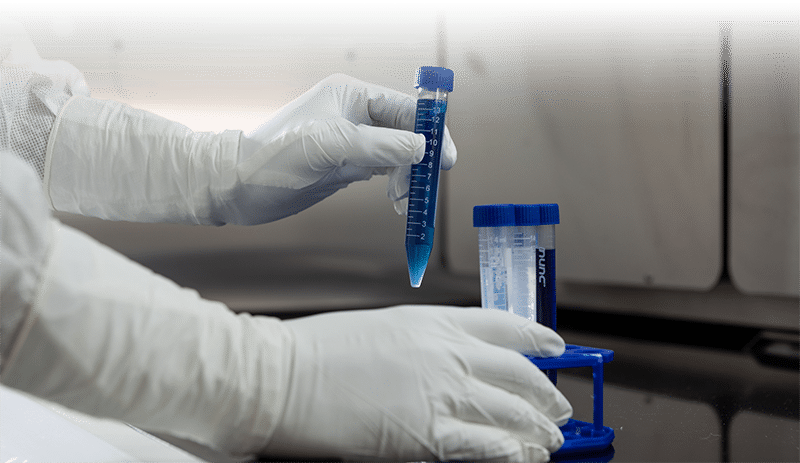
For a cleanroom facility to be classified as sterile, it must be completely free of microorganisms and undergo processes to kill all bacteria and living organisms. In order to maintain cleanrooms’ sterility, aseptic process must be used. The creation of a sterile environment typically means there is no human contact, and aseptic processes are put in place to maintain sterility once humans and other materials become involved. Best practices for maintaining both sterile and aseptic cleanroom facilities include using proper temperature and humidity controls, air filters and installing easily cleaned floors, walls, ceilings and counters. An often overlooked but critical element to help maintain aseptic processes and prevent cleanroom contamination is the usage of proper personal protective equipment (PPE), including disposable sterile gloves. With staff coming in and out of cleanrooms, there is a lot of opportunity for particles, such as dust and other airborne organisms, to be introduced into the cleanroom environment. Therefore, aseptic processes must be incorporated to keep a cleanroom functioning with the proper controlled attributes.
To minimize contamination, cleanroom PPE needs to be manufactured using specific processes that cut down on chemical exposure and control the number of particles and extractables. HALYARD* PUREZERO* Nitrile Gloves are manufactured using a clean process, meaning they are washed repeatedly in deionized water. They are designed to ensure consistent control of lower particles and extractables and are recommended for use in ISO Class 3 or higher and Grade A/B/C/D cleanrooms. Additionally, the HALYARD* PUREZERO* Nitrile Gloves have an accelerator-free formulation, which reduces the risk of allergies and skin irritation associated with accelerator chemicals in other nitrile gloves.
Utilizing both sterile and aseptic processes is key to avoiding any contamination breach that could compromise already completed work or lead to a shutdown for cleaning and re-certification. Focusing on both ensures cleanrooms maintain a stable environment that is mandated for the important work that occurs within them. While the cleanroom makeup and build are important parts of maintaining this environment, ensuring cleanroom employees have access to proper PPE is equally necessary. Proper PPE includes specially manufactured cleanroom gloves and an understanding of the importance of reducing contamination, increasing protection and the best practices for doing so. Together, through proper cleanroom makeup and ensuring the necessary PPE is available, facilities can keep cleanrooms contamination free and most importantly, clean.